Reproductive health care is becoming increasingly hard to access in British Columbia as clinics move to online services and pandemic restrictions make leaving the house more perilous for those seeking care.
Surgical abortions in hospitals, which accounted for about one-third of abortions in B.C. in 2018, continue unaffected by provincial measures to cancel non-urgent surgeries to free up hospital beds.
But health care providers are scrambling to provide contraception, STI testing and medical abortions to those most in need as options for transportation and privacy at home diminish.
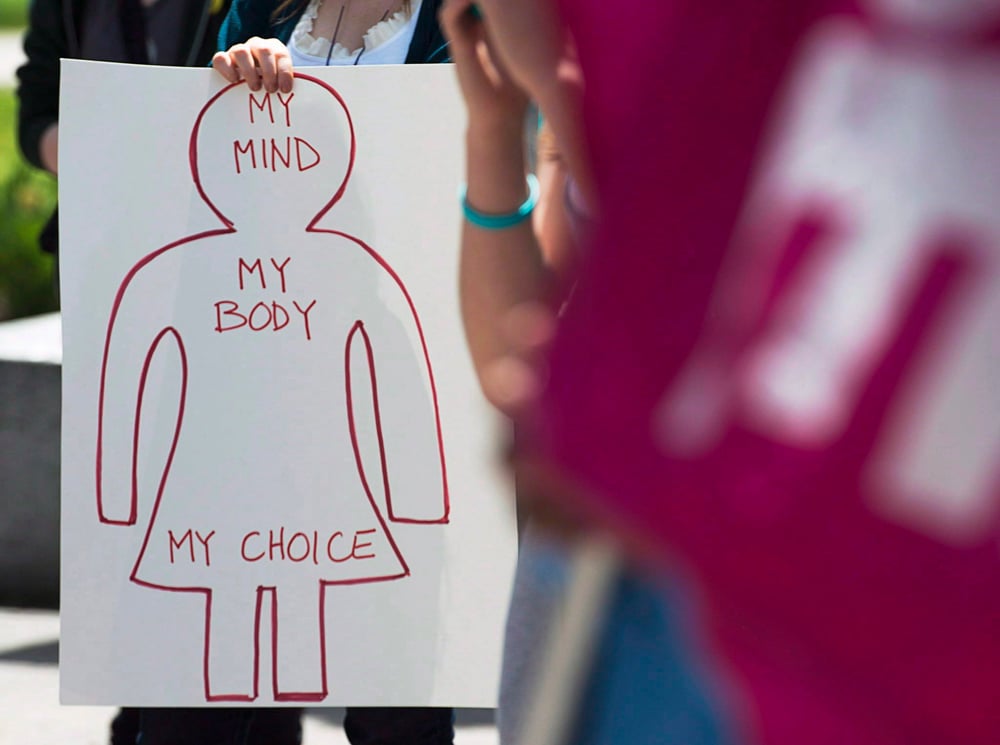
“We have to continue to be an essential service,” said Nicole Pasquino, clinical director of Options for Sexual Health, a non-profit network of reproductive health clinics. “Women deserve this right to have care and to choose to have it.”
Some of the approximately 60 clinics around B.C. operated directly or in partnership by Options have been converted to COVID-19 testing clinics, Pasquino says.
All remaining clinics are open but closed to most in-person visits, except in the case of emergencies or on a case-by-case basis for IUD insertions and other necessary procedures.
But even so, Options is seeing a decrease in people seeking care due to fear of being at risk during an in-person visit or having to go pick-up a prescription from the pharmacy.
Low-cost contraception, like Options provides, are also important as unemployment climbs and people may be faced with tough decisions about whether or not to refill a prescription or put food on the table, Pasquino says.
“Having to make those decisions can really impact a person’s choices in life,” she said. “And it disproportionately impacts women and all folks who need access to contraception.”
Most clinics have switched to telehealth visits, writing and renewing prescriptions over the phone or video, and giving medical advice from a distance where possible to mitigate the risk.
But some are more easily delivered online than others.
Medical abortions, which made up 35 per cent of abortions in B.C. in 2018, are done using a drug called Mifegymiso, the commercial name for two oral medications, mifepristone and misoprostol, that terminate between 94 and 98 per cent of pregnancies safely.
The medication became available in 2017, and Willow Clinic in Vancouver started doing telehealth medical abortions soon after. Consults are typically done over the phone and each patient has a counselling session to talk about their feelings around the procedure.
Under normal circumstances, it’s an efficient way for people who can’t find a service provider in their local communities to access an abortion. Necessary ultrasounds and bloodwork can be completed at local labs, and then once a Willow doctor prescribes Mifegymiso, the medication can be couriered to the woman’s door.
But under current conditions with many labs closed and people hesitant to go outside, clinic executive director Cheryl Couldwell says telehealth abortions are far from ideal.
“It’s not the absolute gold standard of care that we want to give,” she said, noting that doctors need to go further into a patient’s medical history to ensure they have sufficient hemoglobin for the pill to work if labs aren’t available. “It would be much better if we were getting an ultrasound and the bloodwork ourselves.”
But many people still rely on telehealth abortions in regular times due to lack of service providers in their communities or hesitancy by physicians to prescribe the relatively new medication.

While the pill was heralded as a huge step to overcome barriers to abortion access in rural and remote areas, a 2019 Globe and Mail investigation found that that at least 69 per cent of prescriptions for Mifegymiso are issued by clinics in large urban centres across Canada.
Couldwell says some family physicians may feel unfamiliar with how the pill works or how to best support someone seeking an abortion.
Stigma around abortion and not wanting to seek care from a familiar doctor or nurse practitioner in a small community might also drive people to seek out the Willow Clinic or others like it.
In the current pandemic, proper reproductive health care becomes even more essential, Couldwell said.
“There are people at home who may have been thinking of getting pregnant and now they or their partner don’t have a job,” said Couldwell. “To have that added stress of worrying about an unwanted pregnancy when there’s really not a whole lot to do, people don’t need that.”
“We need to be able to offer them whatever they need.”
And access to care has always been particularly important in rural and remote communities, Pasquino says. She worries about the people in communities where Options clinics are their only choice, and where in-person support can mean a world of difference.
“For some people, access to contraception is vital to daily survival,” said Pasquino, noting that survivors of sexual assault need access to medication and contraception as soon as possible.
Those experiencing intimate partner or domestic violence may not have the privacy at home for a virtual visit, as their partners or family may not know or approve that they are using contraception. “In-person support for reproductive healthcare is so important,” said Pasquino.
Joyce Arthur, executive director of the Abortion Rights Coalition of Canada, says the pandemic is exacerbating abortion access issues, particularly as transportation options for women in rural and remote communities to get to clinics are limited.
“It certainly shines a light on existing barriers in the province and it could be an opportunity to remove them,” she said.
One step could be adding telehealth billing codes for doctors in provinces that don’t yet have them and expanding the number of clinics that provide telehealth medical abortions.
Ensuring that people have access not just to abortion and contraception, but to care that suits their needs, isn’t something that can wait until after the pandemic subsides.
“We’ve seen a lot of people make difficult decisions about their reproductive health during these times,” said Pasquino. “Unplanned pregnancies don’t take a break in COVID-19.” ![]()
Read more: Health, Coronavirus, Gender + Sexuality















Tyee Commenting Guidelines
Comments that violate guidelines risk being deleted, and violations may result in a temporary or permanent user ban. Maintain the spirit of good conversation to stay in the discussion.
*Please note The Tyee is not a forum for spreading misinformation about COVID-19, denying its existence or minimizing its risk to public health.
Do:
Do not: