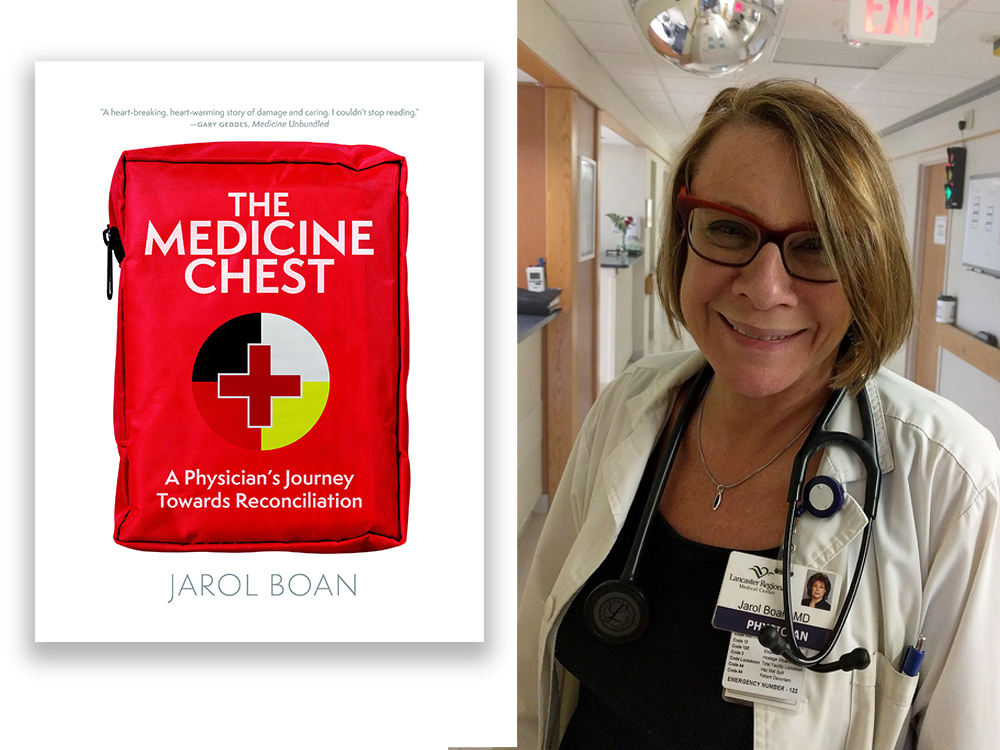
[Editor’s note: Though Dr. Jarol Boan grew up in Regina, Saskatchewan, she spent 20 years treating patients and working in academic institutions south of the border before deciding to return to her home province. ‘The Medicine Chest: A Physician’s Journey Towards Reconciliation,’ excerpted below, documents Boan’s shift towards focusing on Indigenous health once she moved home.
Learning from her Indigenous patients, she began to understand why mainstream approaches to medicine were so often failing them — and what she as a physician should be doing differently. Including examining her own biases. Boan’s portraits of individual patients in the book, except when otherwise noted, have been built from multiple experiences. The names in the excerpts below are pseudonyms.
Content note: The excerpt mentions violence against Indigenous women and girls.]
The elevator door opens, and I walk out into a long corridor. I’m still feeling that this hospital is new to me. I’m not settled in. My thoughts are scattered. I’m focused on getting home after work and making an overdue phone call to a friend in Lancaster, Pennsylvania, 3,000 kilometres away.
Ahead of me I hear the voice of a woman, agitated, shouting in Cree. Outside, it is a bright, cold, windy fall day. The city rolls away from the hospital in every direction, the legislature and the most affluent streets in the south and east, the railway tracks and the poorest districts to the north. Surrounding it all is the south Saskatchewan plain: flat, almost treeless, drawn into neat grids of roads, fences and cultivated farms. Harvest is in full swing and the crops are golden. Inside, everything is beige or stark white with fluorescent light. Neutral. Antiseptic.
Institutional.
I enter the room where my patient waits. She is sitting up in bed, picking at something in the air, dark eyes blazing. Her husband and middle-aged son are sitting on institutional chairs close by, wearing tired, forlorn faces. The patient calms somewhat when I enter the room in my uniform — the white lab coat, the stethoscope.
“Mavis, do you remember meeting me last night?” I ask.
Her eyes harden, and I see a serpent eating at her soul. “You are the devil,” she says. The previous evening, she was coherent but far away, telling me in clipped English that she was crossing a field on the prairie, walking with her father, watching the buffalo. Now she has grown intense, and she is angry with me.
Mavis arrived from her reserve in the Touchwood Hills late on the previous day, a frail woman in her mid-70s bundled into an ambulance, driven for two hours, and deposited in the emergency room with a dangerously elevated INR at 28.1.
INR is the international normalized ratio, which measures the effect of anticoagulants on the clotting system. It is usually used to measure the effect of warfarin, an oral anticoagulant, on the thinness of the blood.
A normal INR level is 1, or between 2 and 3 for patients on anticoagulants; a level as high as 28 is often associated with death from internal bleeding. A CT scan of her head, performed after she was admitted, showed no obvious bleeding in her brain to explain the confusion. I ordered reversal agents to thicken the blood, and this morning her INR indicated normal clotting.
We have fixed the cause of her abnormal blood tests, but she is not better. She is now my patient, and I need to consider how her anger might be related to her medical symptoms. She has heart disease with atrial fibrillation. Thinning the blood to prevent a stroke was what I judged to be the appropriate treatment for her heart disease, but it may be that the treatment has become life-threatening.
In order to heal her, I have to understand why her blood was so thinned in the first place. Was it alcohol use, kidney failure, confusion about dosing, a suicide attempt?
I turn away from Mavis as she fends off the serpent inside her, and I focus on the family at her bedside. Her husband is a heavy-set man wearing a beaded jacket and blue jeans, his long greyish hair in a braid down his back. He tells me he is an Elder on the reserve and does pipe ceremonies. They have been married for many years.
He says she has been taking her heart pills regularly, but there is no evidence she intentionally took too many. Checkmark: strike suicide attempt off the list. She is not a drinker. Checkmark: strike alcohol interaction with her pills off the list. From a review of her blood work in the hospital chart, I can see her kidneys are working well. Checkmark: strike kidney failure off the list.
Still, she is sick, and she is angry. I suspect that she has every reason to be angry, aside from her illness, although I have never experienced racism or real deprivation myself. I grew up in a comfortable home, surrounded at school by white faces, steeped in a culture that celebrated the bravery and enterprise of the early settlers — the men and women who broke the soil, the doctors and police officers. As I passed through college in the early 1970s, a truer perspective started to emerge. I learned about the Canadian government’s treaties with Indigenous Peoples in Saskatchewan.
Shortly after the time of Canadian Confederation, the Hudson’s Bay Co. transferred the governance of Rupert’s Land to the government of Canada, under pressure from Great Britain, for a price. Through two centuries of fur trading, the Hudson’s Bay Co. had transformed the pattern of economic activity among Indigenous people, but the land stretching from the Pacific coast through much of what is currently Ontario still lay open for traditional use. There were no police or government agents in the early fur trading days.
On July 1, 1867, the British North America Act created the Dominion of Canada, a self-governing entity within the British Empire. Suddenly, the Crown appeared, in the form of an Ontario-based Conservative government, intent on transforming the prairies into a replica of southern Ontario. The treaties, along with the Indian Act, were the government’s key instruments in clearing the land for settlement. Through Treaty 4, the Canadians seized the field where Mavis, in her visions, watched buffalo.
They carved up the prairie landscape and put Mavis’s people on reserves. Treaty 4 was signed by her ancestors at Fort Qu’Appelle in 1874 — two years before Custer’s Last Stand, the Battle of the Little Bighorn, in what is now the state of Montana. Over a century later, the Truth and Reconciliation Commission called this process of treaty-making part of Canada’s “cultural genocide.”
It is an indication of the strength and resilience of Indigenous people like Mavis that they have survived and often showed a talent for succeeding in the world that was forced upon them by settlers intent on westward expansion. Saskatchewan’s Poundmaker reserve was the birthplace of Hollywood star Gordon Tootoosis; the Red Pheasant reserve was home to the accomplished Indigenous artist Allen Sapp; and Maria Campbell, who became a lifelong advocate for Indigenous arts and politics, was born on a trap line in northwestern Saskatchewan.
The Chief from Mavis’s homeland in the Touchwood Hills was party to signing Treaty 4 in 1874. He remained Chief of his band until his death nearly 20 years later.
When the treaty was signed, the Chief and his council carefully chose heavily wooded land to give them access to wild game and firewood in the harsh prairie environment. Cultivation was done at that time using spades and hoes; a plot known as the “community garden” was maintained by the whole reserve. The community developed a fine herd of cattle, each farmer keeping his herd until it numbered 10 to 12 heads, and then giving half of the animals to someone else who could then get started. After the band received walking ploughs, its members began to grow wheat, barley and oats; with the arrival of the railway in the early 1900s, an outlet was created for the sale of their produce. In the 1940s, the band purchased their first tractor.
They worked hard on a cramped piece of land that was less than ideal for farming, and they persevered. The “white chiefs” had promised a “medicine chest” in Treaty 6 signed at Fort Carlton in 1876, but the federal government’s health-care efforts in the first half of the 20th century were less than minimal. Indigenous children were taken, some at gunpoint, to live in residential schools where they risked death from tuberculosis, other infectious diseases, starvation and abuse. Housing on reserve was provided rarely and unpredictably, with no resources for maintenance.
Using my medical skills and training, I conclude that Mavis is suffering from white matter disease and explain my findings to her husband.
The brain has several parts — the grey matter is where cognitive functions happen, and the white matter is the connective fibres that link the various parts of the brain, just as a railroad track connects two cities. Mavis’s CT scan indicates that she has evidence of small vessel disease in the brain that is associated with dementia, balance problems and difficulty with multitasking. It worsens with infection or stress. It is likely that as her mild dementia tipped over into severe dementia, she was unaware of the progressive decline and mistakenly took too many of her pills, which would explain why her blood was so thinned.
There is no treatment for white matter disease, except to improve the underlying stressful situation. With rest, good nutrition, controlling blood pressure and exercise, the symptoms improve with time. Her husband accepts my explanation but does not seem convinced that she will improve.
Over the next short while I return to Mavis’s room daily. Her husband sits by her bedside for three days. She grows stronger and interacts with the staff and me. Her son is also visiting. Her daughter flies into Regina from her job in Toronto.
On the fourth day she is alone. She smiles at me, is well groomed and sitting comfortably in bed. Her blood work has normalized, and she is calm in her speech. Her caring family has disappeared. And she is alone. Where have they gone?
I begin to suspect a case of “granny dumping.” This term was coined in the 1980s by medical professionals who observed relatives dropping off the elderly in emergency rooms when the family was unable or unwilling to care for them due to burnout or lack of financial resources. Granny dumping typically peaks before long weekends and at Christmas. It is spoken of as a widespread condition in the health-care system; it creates a dilemma for physicians and social workers reluctant to discharge a patient when a family is absent or doesn’t show up for meetings with the hospital staff.
I become convinced that this pleasant family has hoodwinked me. I had thought they cared for Mavis. I feel irritation with myself at my blind trust.
Four days later, Mavis’s husband reappears. I find him sitting calmly by her bedside. I hide my irritation and respond to him carefully and professionally. I explain that she has improved further and will soon be ready to go home. We are waiting for one last test on her heart. She will likely be discharged tomorrow. I ask her husband, “Are you okay with that?”
He smiles gracefully with this news. Then he looks me in the eye and says, “I’m sorry that I couldn’t be here for the last few days. We had a crisis on reserve. One of our young girls was found in a ditch after being raped and killed. We had religious services to honour her.”
I am embarrassed and ashamed. I had been caught up in my privileged view of appropriate behaviour while the community on reserve was grieving the loss of one of its youth and reeling in the face of the violence against her. He tells me that the culprits were likely non-Indigenous, the details are fuzzy, and no one has been caught yet.
I had fallen into the trap of making assumptions about Indigenous people and granny dumping. I am on a path of discovering my own racism.
Adapted from ‘The Medicine Chest: A Physician’s Journey Towards Reconciliation.’ Copyright 2024 by Jarol Boan. Reprinted by permission of University of Regina Press. ![]()
Read more: Indigenous, Health, Books, Rights + Justice















Tyee Commenting Guidelines
Comments that violate guidelines risk being deleted, and violations may result in a temporary or permanent user ban. Maintain the spirit of good conversation to stay in the discussion and be patient with moderators. Comments are reviewed regularly but not in real time.
Do:
Do not: