[Editor’s note: This article is part of a Tyee partnership with Victoria-based Hakai Magazine, which is publishing stories about COVID-19 in these pages during the pandemic.]
For health officials, fast and accurate testing for COVID-19 to contain and stop the spread is one of the main goals behind the viral detective work being done on the novel virus.
Decisions on testing, both selective or widespread, will be a key factor in deciding when and how to remove restrictions for the public and reopen workplaces again, say business leaders. Scrambling to set up a stable supply chain of necessary components for testing, British Columbia provincial officials have collaborated with private industry to get the job done.
“It’s been a team effort,” said Andrew Wynn-Williams, divisional vice president for Canadian Manufacturers and Exporters. “As ever when you’re working with a big organization like government, things could always be speedier, but I’ve really been impressed with how it’s been managed.”
He praised the B.C. government for its quick creation of the COVID-19 Supply Hub website, which functions as a centralized access point to match suppliers with needs.
B.C.’s biotech industry is playing a part as well.
“Rallying our community has not been hard. They are generous, smart and action-oriented,” said Wendy Hurlburt, president and CEO of LifeSciences BC, an industry association representing the biotech sector.
In early March, LifeSciences BC redistributed supplies — such as personal protective equipment — and now members help match experts with needs, whether it is identifying lab space or converting manufacturing facilities to produce PPE, while they continue to work with the province on sourcing essential items. The current situation has revealed weaknesses in the health-care system, including the lack of a sustainable supply chain for made-in-Canada critical care items. Canadian manufacturers are kicking into gear, but that supply chain should be maintained even after the COVID-19 pandemic passes, Hurlburt said.
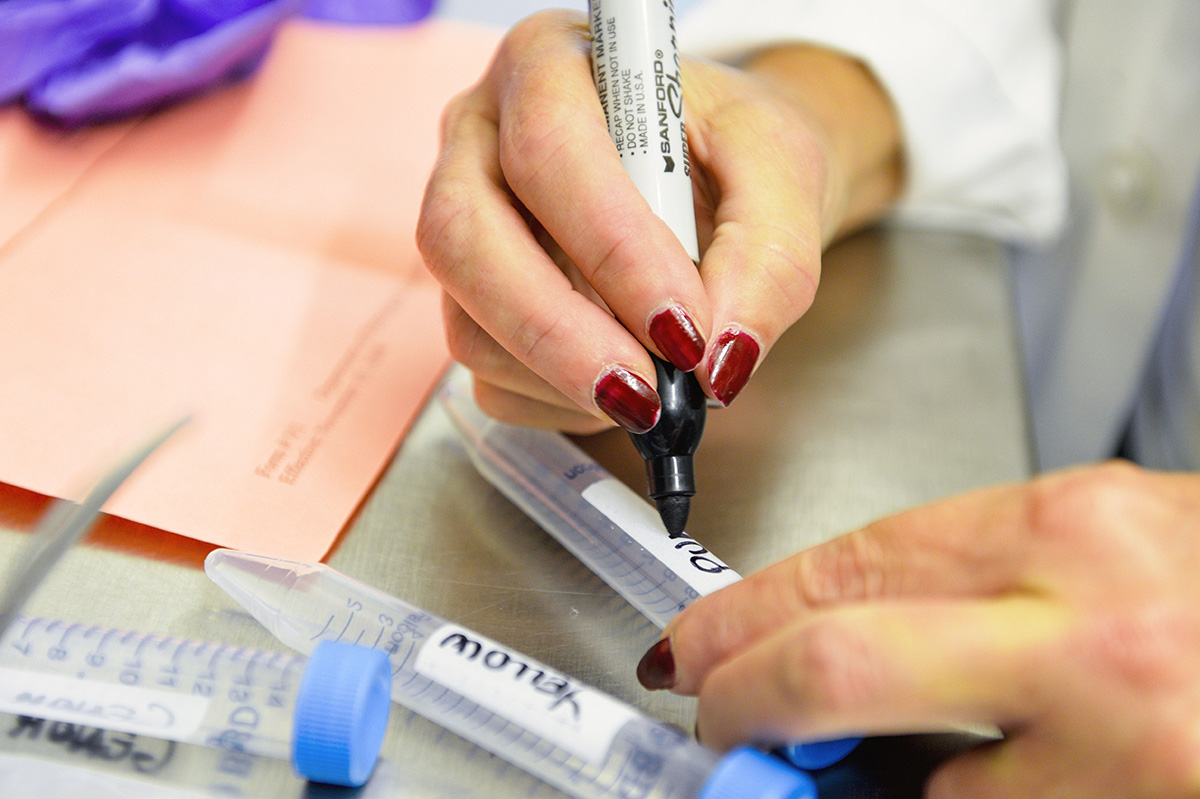
Tests to confirm a diagnosis of COVID-19 are of most importance right now.
The press for quick turnaround tests
Health Canada has approved a range of diagnostic tests so far, with more products awaiting approval. Most are lab-based in which swab samples are sent to private or hospital labs for processing. Although labs can process large volumes of tests, patients in outlying areas may wait a day or more for results. But rural regions with smaller urban centres need quick results to manage the outbreaks, say the experts. Ontario company Spartan Bioscience has developed another option (approved last week) to produce a portable and fast COVID-19 test. Results from the throat or nose swab samples can be produced in an hour, a boon to remote communities far from labs. The company quickly received large orders from Quebec, Ontario and Alberta.
Dr. Bonnie Henry, British Columbia’s provincial health officer, said the province will use another method to test people in rural regions. The province has several rapid molecule diagnostic machines called GeneXperts, a proven 20-year-old technology that is used to test for tuberculosis, influenza, strep and other diseases. The strategy is to deploy these machines to areas of the province where turnaround time is an issue, said Henry.

British Columbia has enough of a test supply right now to handle the province’s seek-and-trace testing strategy that focuses on certain groups such as health-care workers, long-term care residents, and other groups vulnerable to complications due to COVID-19.
“The percentage of positive tests has been going up which tells us that we’re finding the people we need to find,” said Henry at a daily briefing, adding that as the flu season comes to an end, doctors are seeing fewer people with similar respiratory symptoms. That said, British Columbia is also doing surveillance testing; meaning that any samples sent to the lab from people with other respiratory problems will automatically be tested for COVID-19.
According to some doctors, however, our selective testing offers us only a partial view of the situation. “We need to test more of the iceberg,” said Dr. David Forrest, an infectious diseases specialist and critical care physician at Nanaimo Regional General Hospital. “We’re not finding the minimally symptomatic.” Although he expects a surge to come eventually, he said. Nanaimo has been spared so far, which he suspects is due to more people living in single-family homes rather than high-density housing. And he can send tests to labs in Victoria and have them back within 24 hours.
Strengthening virus-fighting supply chains
At the national level, industry groups and government agencies are working hard to supply virus screening tests, vaccines, therapeutics and symptom management treatments even as the pandemic continues to strain global supply networks. On March 25, the non-profit organization Next Generation Manufacturing Canada announced a $50-million fund for projects that can lead to the rapid production launch of critical equipment and supplies to support Canada’s COVID-19 response.
In addition to managing project funding, NGen is working through its network of members to identify manufacturing capabilities that can scale and expedite the manufacture and distribution of diagnostic test kits and auxiliary components like nasal swabs.
Although new products are being readied for mass production, the research continues on alternatives. The Public Health Agency of Canada and the National Research Council of Canada are sponsoring a competition for funding to create a home-based testing kit costing under $40 that provides easy-to-understand results in 20 minutes. The deadline for applications is April 20. At the same time, about 100 research programs have been approved under the Canadian 2019 Novel Coronavirus Rapid Research funding opportunity.
Microbiologist Horacio Bach, adjunct professor in the division of infectious diseases in the UBC Faculty of Medicine, is one of 14 researchers in British Columbia to receive funding as part of the federal rapid research program to fight COVID-19 by finding new therapeutic options or diagnostic tests.
Bach’s project will explore how to design antibodies that neutralize the virus and block its ability to enter cells. “In order to multiply, the virus has to go inside the cell and once it hijacks the machinery inside, the cell starts to produce only viruses. If I can provide something that blocks the virus from going from cell to cell, I will buy time for the body to recover. I will be looking at several parts of the protein used by the virus when it invades the cell,” Bach said. He will validate results using blood plasma from recovered COVID-19 patients, but getting that material takes time as it goes through ethical approvals at several levels.
The true picture of infection rates won’t be visible until antibody tests are distributed widely. And it could be months before those new products are ready. Antibodies in the blood indicate the body’s reaction to a previous illness. While this retrospective view can do little for those suffering the symptoms, these test results can make it easier to plan for lifting the physical distancing restrictions and business closures currently imposed. A randomized test in Iceland showed that 50 per cent of the people who tested positive for antibodies for COVID-19 had never had any symptoms. So the testing results here could be enlightening.
Blood tests: last puzzle piece
The serology (blood) tests for antibodies are the final piece of the puzzle — they are simple to administer and similar to a blood glucose test. Already used in other countries, the tests, including a product from Canadian company BTNX Inc., have not been approved yet in Canada.
The blood test would mean a great deal to businesses struggling for survival right now. A testing strategy that allows employees to receive a health certificate showing they’ve had the disease could be the ticket to economic recovery. “If you have immunity you could go back to your employer with confidence,” said Val Litwin, president and CEO of the BC Chamber of Commerce. He added that an assurance of safety through careful testing would help get people working again.
Testing results can be a critical tool for health officials as they manage the outbreaks. Public pressure to bring new tests to market quickly has been intense, but questions about the accuracy and sensitivity of tests — both the nasal or throat swabs and the blood antibody tests — have made B.C. health officials cautious about relying solely on this data. Swab tests to identify COVID-19 in a patient can give false negatives, sometimes due to the method of sampling or handling before it reaches the lab. The swab tests can be less accurate for people with mild cases or no symptoms at all. Blood tests to check for immunity after people have had the disease may turn up false positives by identifying other coronavirus antibodies associated with the common cold.
For now, directives such as social distancing, isolation and handwashing are still as important as widespread testing for health officials’ management strategies. ![]()
Read more: Health, Coronavirus, Science + Tech















Tyee Commenting Guidelines
Comments that violate guidelines risk being deleted, and violations may result in a temporary or permanent user ban. Maintain the spirit of good conversation to stay in the discussion.
*Please note The Tyee is not a forum for spreading misinformation about COVID-19, denying its existence or minimizing its risk to public health.
Do:
Do not: