Compiled by veteran medical journalist Brian Owens, this roundup of some of the newest science on the COVID-19 pandemic, straight from the scientific journals, is presented by Hakai Magazine in partnership with The Tyee.
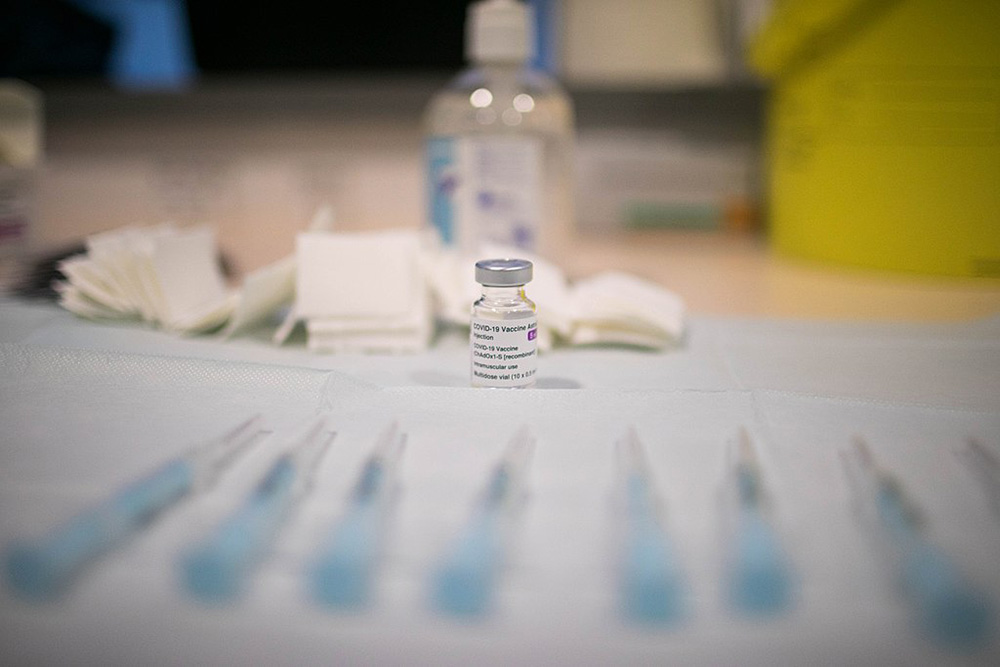
Risk of blood clots from AstraZeneca vaccine quantified
There is a real, but low, risk of blood clots in the veins, including in the brain, after immunization with the AstraZeneca COVID-19 vaccine, according to a large study in Norway and Denmark. The study looked at 280,000 people in the two countries who received the first dose of the AstraZeneca vaccine, and compared the rates of clot with those expected in the general population. They found 59 blood clots in the veins compared with 30 expected, corresponding to 11 excess events per 100,000 vaccinations. But they found no increase in the rate of arterial clots, which can cause heart attacks or strokes. The researchers and public health officials say that in most cases the benefits of the vaccine outweigh the risks.
The British Medical Journal, May 5, 2021
Pfizer vaccine protects against asymptomatic infections
Vaccination with the Pfizer-BioNTech dramatically reduces the risk of both symptomatic and asymptomatic infections from COVID-19, according to two studies of health-care workers in the U.S. and Israel. In one study, conducted at St. Jude’s Research Hospital in Memphis, Tennessee, vaccination reduced the risk of asymptomatic and symptomatic SARS-CoV-2 infection by 79 per cent compared with unvaccinated employees. An analysis of asymptomatic infections alone found vaccination reduced the risk by 72 per cent. Protection was even greater after receiving both doses of the vaccine.
Journal of the American Medical Association, May 6, 2021 (1)
Journal of the American Medical Association, May 6, 2021 (2)
Novavax vaccine works against South African variant in trials
The COVID-19 vaccine made by Novavax has shown strong protection against the B1351 variant that was first identified in South Africa in phase two clinical trials. The trial found that the vaccine provides good protection against mild disease caused by the variant, and 100 per cent protection against severe disease. This vaccine has not yet been approved for use anywhere.
New England Journal of Medicine, May 5, 2021
How to predict the severity of a COVID-19 infection
The severity of a COVID-19 infection can vary widely between patients, with some experiencing almost no symptoms and others requiring ventilation in the intensive care unit. Predicting which path a patient is likely to take would help doctors better plan their care, so researchers have been hunting for biological markers that might help make that prediction. Two groups have now found promising candidates, both of which are related to our body’s immune response. One group found that levels of an inflammatory immune protein called interleukin-6 rose steadily in patients who died, while it rose and then fell in patients who survived. The other group found that patients with lower levels of natural killer T cells, a cell involved in the early stages of the immune response, tended to have more severe disease.
Cell Reports Medicine, May 4, 2021
Risk factors for outbreaks in retirement homes
For retirement homes where residents are more mobile and independent, size, location, number of services offered, and whether a home is part of a chain are all risk factors for COVID-19 outbreaks, according to a study of 770 homes in Ontario. Larger homes had a three-fold higher risk of an outbreak, and those that provided nine or more different services had a 2.5-fold higher risk, likely because of the number of staff coming in and out. Being part of a chain, sharing facilities with a long-term care home, and being in an area with a larger ethnic minority population also increased the risk of an outbreak.
Canadian Medical Association Journal, May 10, 2021
Obesity is a bigger risk factor for men
People who are obese are at higher risk of severe disease and death from COVID-19, but the risk appears to be greater for men than for women. An analysis of more than 3,500 patients found that both moderate and severe obesity were associated with more severe disease and risk of death in men, but the same was true only of severe obesity in women.
European Journal of Clinical Microbiology and Infectious Diseases, May 6, 2021
Struggling students benefit most from online learning
Students who were struggling academically benefited the most when schools switched to online learning at the beginning of the pandemic, and there was no detrimental effect on high achievers, according to a study of schools in China. But the quality of the teachers preparing the online lessons had a big impact on student outcomes. Another study of students in China identified the different needs of students at different ages. Younger children need guidance from teachers and parents, while older students require more opportunities to collaborate. Both studies also found that many students were engaging with online learning through mobile phones, which was linked to poorer results.
China Economic Review, May 2, 2021
British Journal of Educational Technology, May 4, 2021

How good were the experts’ early pandemic predictions?
Experts such as epidemiologists and statisticians made more accurate predictions than the public about the course of the COVID-19 pandemic, but both groups substantially underestimated its true extent. In April 2020 researchers asked experts and the public in the U.K. to make predictions about the impact of COVID-19 by the end of 2020, such as the number of deaths and infection rates. Both groups underestimated the total number of deaths and infections in the U.K. The official U.K. death toll on Dec. 31 was 75,346. The median prediction of the expert group was 30,000, while the median prediction for the non-expert group was 25,000.
Ibuprofen does not increase the risk from COVID-19
The use of non-steroidal anti-inflammatory drugs such as ibuprofen does not lead to higher rates of death or severe disease in patients who are hospitalized with COVID-19, according to a new study of more than 72,000 people in the U.K. Early in the pandemic there was some concern that the use of these drugs, commonly used to treat conditions like acute pain and rheumatoid arthritis, could increase the severity of COVID-19. But the study found that people who had used NSAIDs before being admitted to hospital were no more likely to die from COVID-19 than those who had not used the drugs.
The Lancet Rheumatology, May 7, 2021
Young, healthy people can still have long-term effects
Young, relatively healthy people who had only a mild case of COVID-19 could still have long-term cardiovascular complications from the disease and be at higher risk of future heart problems. Researchers found increased stiffness of the arteries, including the carotid artery that supplies blood to the brain, in a study of young COVID-19 patients, indicating they may have increased risk of cardiovascular complications for some time after their infection.
Experimental Physiology, April 26, 2021 ![]()
Read more: Coronavirus, Science + Tech















Tyee Commenting Guidelines
Comments that violate guidelines risk being deleted, and violations may result in a temporary or permanent user ban. Maintain the spirit of good conversation to stay in the discussion.
*Please note The Tyee is not a forum for spreading misinformation about COVID-19, denying its existence or minimizing its risk to public health.
Do:
Do not: