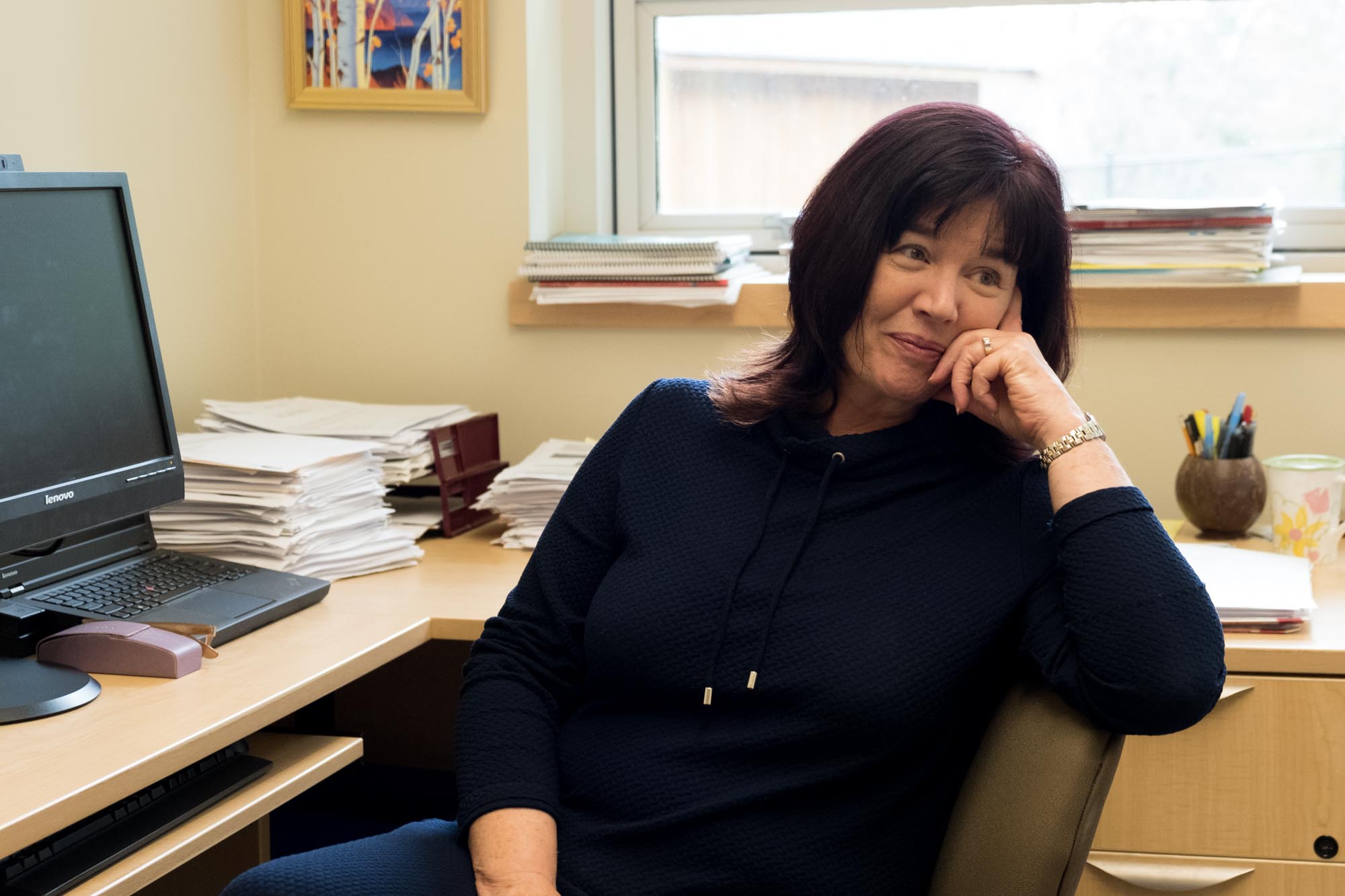
Shaila Misri was finishing her residency at Vancouver General Hospital in 1978, working long hours in the obstetrics ward, when she noticed something troubling.
The women who came into the ward with physical problems were identified right away, and doctors and nurses were quick to assist them.
But mothers with clear symptoms of depression or anxiety weren’t getting any treatment. “I thought, something has to be done about that.”
It was a decision that led to a change in career for Misri — and to a revolution in care for pregnant women, new mothers and their families.
Misri, at 30 years old, decided to train to become a psychiatrist and focus on the mental health needs of new moms.
Then, as now, our culture presented pregnancy, childbirth and the early days with a new baby as a series of warm and happy moments. But that’s far from the reality for many women and families.
“There are aspects to childbirth and pregnancy fraught with a lot of mental health issues and struggles that nobody talked about,” said Misri. Because they weren’t discussed, women were reluctant to seek help, or unable to recognize they needed it.
And if they did, Misri recalled, they were treated in the same ways and same places as severely ill psychiatric patients.
She quickly realized that mothers and their babies needed specialized care that simply didn’t exist. “There was physical help, there was medical help, but there was no psychological help,” she said.
Misri said she began campaigning within the hospital for a dedicated mental health program around pregnancy and childbirth.
“I started just going to the women’s hospital when I was on call, voluntarily,” she said. She would tell the maternity ward staff she was available to help women in crisis.
She was a fully qualified psychiatrist, but she decided she would keep doing this work without pay until she could prove there was a need.
It didn’t take long. After giving birth to her own child in 1983, Misri got a call from the hospital.
“I was asked to come rescue a very sick bipolar mom. Day two or three postpartum, and she was really ill, she was psychotic,” Misri said. The people in charge of obstetrics asked Misri that night: “‘What does it take for you to start this program? We need your help.’”
And so the Reproductive Mental Health program began at BC Women’s Hospital. Misri’s office was in a room stuffed with beds that residents and doctors on overnight shifts used for naps, she said.
Within six months she had a waiting list. Each patient she saw seemed to bring in three more. She hired a second psychiatrist, Dr. Diana Carter.
Together they built the global standard for mental health care around pregnancy and childbirth. And learned how to press politicians for change.
“Back then, if you had an idea as a physician, you could fly to Victoria and talk to people,” said Dr. Deirdre Ryan, who has been a psychiatrist at Reproductive Mental Health for over two decades and took over from Misri as the medical director in 2018.
“We were able to actually talk directly to people and say what’s happening, this is what we need. Those days are over. Those days are well gone.”
At the time, postpartum depression wasn’t even recognized as an illness. It wasn’t until 2013 that the DSM-5 — the diagnostic manual of mental disorders — added postpartum depression for the first time.
The long delay was costly.
“If there are no criteria to describe it, who is going believe that it exists? Who’s going to give you money for research?” said Misri. “And who’s going to give you treatment?”
Today, the BC Women’s Hospital Reproductive Mental Health program includes a multidisciplinary team of over a dozen people, including psychiatrists, counsellors, a couples’ counsellor, a social worker, a dietician and a nurse clinician.
The team cares for around 5,000 patients a year, consults with physicians around the province, offers telephone appointments for patients in rural areas, hosts video-based training for professionals, and trains other hospitals to set up their own perinatal mental health treatment teams.
The program plays a critical role in a distressed new mother’s care, said Sheila Duffy, who leads the Pacific Postpartum Support Society, a peer-support network for new mothers experiencing postnatal anxiety or depression.
“Their clinical expertise is essential for many of the moms we support,” she said. “Having worked closely with the psychiatrists there over the years, we know that they are instrumental for so many mothers as well as other care providers to make sure that no family falls through the gaps that often exist when people reach out for help.”
But the program’s impact goes far beyond British Columbia, or Canada.
In 2006, Misri wrote a book, Pregnancy Blues, based on her experience and research. That book would be a lifeline for other doctors, including Dr. Elena Serrano, a psychiatrist in Spain who, in 2011, treated a pregnant patient with depressive symptoms.
“I found it and I followed it,” Serrano told The Tyee from her Madrid-based outpatient clinic. She was able to guide a new mother out of depression. “It went really good.”
Like Misri before her, Serrano saw the need to specialize in postpartum mental illnesses, but there was no training available in Spain. So she arranged to do a three-month residency in Vancouver, at the Reproductive Mental Health program.
The program is the first of its kind in Canada and has become a model. Several hospitals in the Lower Mainland received training from its staff to set up their own teams, and hospitals across Canada and the U.S. now have dedicated perinatal mental health treatment teams.
In Spain, today, Serrano has specialized her psychiatric practice on perinatal mothers and families.
“I’m getting invitations now to speak in countries that I could never imagine that I would,” said Misri. “Also, residents and fellows are coming from Saudi Arabia and places like that where women are not even able to drive a car, never mind get help for having thoughts of harming a baby. So there’s a very big shift.”
What is postpartum depression?
Postpartum depression and anxiety are treatable mental illnesses affecting (mostly) mothers during and after pregnancy. A number of factors — hormonal changes, fatigue, dealing with major life changes — can contribute to onset.
More than 10 per cent of mothers (and to a lesser extent, fathers and adoptive parents) experience postpartum depression. Recent studies suggest postpartum anxiety is even more common, affecting as many as 30 per cent of mothers.
Knowledge of postpartum depression developed slowly in western medicine, with dramatic assumptions and little evidence. The first known mention was Hippocrates’ hypothesis that birth fluid was backing up to the brain, causing mania. Fifteen centuries later, in 1928, a psychiatrist theorized it was the result of “pre-pregnancy frigid personalities” or perhaps unresolved sadist tendencies towards men.
In the 1950s, the phenomenon was called baby blues and, as the name suggests, not taken particularly seriously.
The U.S. Congress passed a resolution in 1999 to propose studying and raising awareness about the illness.
The symptoms vary, but they can be devastating. Postpartum depression might look like a lack of interest in mothering, or hyper-anxiety over the baby’s well being, sometimes to a level of obsessive-compulsive disorder. It can bring oppressive feelings of fear, or a sense that something’s missing in oneself.
Many sufferers have intrusive thoughts — unwanted, vivid images of harming the baby or themselves. Some can’t sleep; some oversleep. And, all the while, they are trying to reconcile their feelings with the social expectation that a baby brings bliss.
Powerful as the symptoms can be, often it’s just within a mother’s ability to hide them, even from family and friends. And many do.
“Twenty per cent of women with postpartum depression have thoughts of harming their baby, OK?” said Misri. “Try and tell that to your doctor. He or she, at the time that I started, would be horrified. They would think you were a bad mother, right? There’s a very great issue of being judged and being stigmatized when you’re ill.”
Misri and her colleagues have been working hard to end that stigma and encourage people to seek help — and to ensure it’s there when needed.
One woman’s story
Angela Vass was 20 weeks pregnant when something went weird. A numbness descended on her and wouldn’t lift. She’d been excited to be pregnant. She and her husband wanted a baby and had planned for it. And yet suddenly Vass felt flat.
Vass is in her mid-thirties with mermaid-style turquoise and purple hair. She and her husband, an electrical engineer, recently bought a condominium in New Westminster.
She still wanted the baby, but medical complications during pregnancy made it feel like her body was betraying her at every turn. She was desperate not to be pregnant anymore.

Her daughter’s birth was induced at 36 weeks, and shortly after, the intrusive thoughts began.
“You know when you’re like standing on the precipice of a cliff or something, and you have that stray thought of like, what would happen if I jumped? Except it seems like you’re always standing on the cliff,” Vass said.
“Driving a car, I’d be like, ‘Man, wouldn’t it be nice if I got hit by a train right now?’ Or like ‘Man, what if I drove into that ditch,’ or ‘What if I drove into that telephone pole?’
“It wasn’t that I wanted to die. I didn’t want to die, and I definitely didn’t want my child to die. But in a weird bizarre way it was like, if I just get in a bad enough accident that I have to go to the hospital for a while, maybe I’ll at least get some sleep.
“It’s not logical. Intrusive thoughts really never are. And it’s not like you’re thinking these things on purpose, they just pop in your head.”
Fortunately for Vass, her friends had been vocal about their experiences with depression.
“Because they were, even though I was in this weird numb grey space, I went, ‘Oh, something is wrong with my brain, I should probably tell my doctor.’”
Armed with an antidepressant prescription, a referral to Reproductive Mental Health and a phone number for Pacific Postpartum Support Society, Vass made it through.
During the four months she was on the Reproductive Mental Health waiting list she worked with a counsellor through the society. The antidepressants helped slow the thoughts down, and group counselling at PPSS taught her that she wasn’t alone.
(Waits for the Reproductive Mental Health program problem vary based on the urgency of the patient’s situation. The program also consults with doctors whose patients are on the waiting list or unable to travel to Vancouver.)
When her daughter was about four months old, Vass started seeing Deirdre Ryan at the mental health program. She had never seen a psychiatrist and recalls being anxious and uncomfortable. But before long, she came to rely on her monthly appointments with Ryan.
“She had a couch in her office and a nice rug. Depending on [my daughter’s] wakefulness, we’d sit on the floor, you know, do some tummy time or something while we were chatting,” she said.
“It wasn’t like a lot of psychiatrist appointments where you’re there for 20 minutes, you talk about a thing, and then they hand you a prescription. It was an hour and a half of talking about what I was feeling, what I was going through. And it wasn’t just restricted to postpartum depression. We talked about issues from my childhood that it turned out were affecting my feelings about things now.”
Reproductive Mental Health takes a multidisciplinary approach to treatment. Vass and her husband attended a workshop that helped partners to understand what going through postpartum depression is like.
Vass was referred to a lactation consultant as well as a dietician when her psychiatrist found out that amid the stress of feeding her baby, Vass wasn’t properly feeding herself. The dietitian made a simple, doable, healthy food plan for Vass.
What works
Cognitive Behavioural Therapy and antidepressant medication are known to be effective treatments, both of which are available through the Reproductive Mental Health program, which is covered by B.C.’s Medical Services Plan.
CBT is a widely used talk therapy treatment that helps patients reframe their thoughts about persistent issues in their lives, which naturally changes their behaviour and reactions to these issues.
But to receive treatment, somebody has to recognize that treatment is needed and know that it’s available. Stigma and social pressures can block the way.
Even when a mother agrees to seek help, treatment depends on the experience and training of the counsellors or medical staff. Patients will often minimize their struggle, or not divulge their whole story.
One Fraser Valley midwife said she refers patients to a hospital without a postpartum mental health team, and often gets reports back to her with a description of what the patient was wearing.
“They say, ‘She showed up with clean hair and modern clothes, she seems OK. No follow up needed!’” But the midwife, who’d tracked with this mother over a period of months, could see that whatever support she was getting wasn’t enough. “We have other patients who are totally well-adjusted coming in all messed up with food on their face. It’s not a measure of depression.”
A teaching clinic
Education is a big part of the work at Reproductive Mental Health. It’s a teaching clinic, so medical students and residents learn about the complexities of assessing and treating perinatal psychiatric illness. When doctors, midwives, counsellors and others are more knowledgeable, patients are more likely to be noticed. Especially the ones who are struggling silently.
They can safeguard, as well, “children who are exposed to moms who are chronically ill,” said Ryan.
Children with depressed mothers are at a higher risk of mental illness themselves, and some studies point to decreased immune responses.
The Reproductive Mental Health team has published a library of resources online to support their teaching and to increase capacity for care in B.C. There are best practice guidelines for health care providers, workbooks, online guides for physicians, an online course for physicians through UBC’s continuing professional development program called Beyond the Blues as well as an online module for public health nurses.
“The main thing is that it’s treatable,” emphasizes Ryan. “We assess women who have never been seen by a psychiatrist before, and who may have been struggling for years, and if they get the treatment they need, they can do better than they’ve ever done.”
Misri is all too aware of the tragic toll the illness still takes when left untreated. She recounts the story of a nurse, married to a family physician, who last year took her life by leaping off of Prospect Point.
“Well, she was a very ill woman. First of all, she didn’t want to go a general hospital. She was admitted [to a psychiatric ward] but was discharged against medical advice, OK, because it was impossible for her to stay in the ward when there were so many other sick people that were not like her. It was very frightening. So, she ran. She left her house and jumped off, because all options were closing on her. Four months postpartum is not a joke.”
Ryan said she and her colleagues want to see every pregnant woman screened for symptoms of postpartum depression. The process merely requires a woman to answer 10 questions. Ideally, it would be done at least twice, once during pregnancy and once a few weeks after birth. Currently, Ryan estimates, about half of pregnant women are screened.
In the push to close that gap, the stakes are high, Ryan said. Left untreated, women with postpartum depression suffer themselves, which in turn “can have adverse effects on the developing child as well.”
“If there’s one message to get across,” she added, “it’s that postpartum depression is common, but it can have serious consequences if it’s not treated. But it is treatable. And with treatment women can do incredibly well and babies do better.” ![]()
Read more: Health














Tyee Commenting Guidelines
Comments that violate guidelines risk being deleted, and violations may result in a temporary or permanent user ban. Maintain the spirit of good conversation to stay in the discussion.
*Please note The Tyee is not a forum for spreading misinformation about COVID-19, denying its existence or minimizing its risk to public health.
Do:
Do not: