I zip up my fleece even as I savour the early morning chill on my face. Bouchie Lake’s water is indigo, swallowing a cloudy sky. Ripples nudge pockets of snow on the banks, winter’s frozen paws grasping well into May.
I don’t mind. It won’t be the first time we have a late spring and it’ll mean less fires this summer.
A neighbour comes out her front door and we wave our greetings. She’s one of my patients and suddenly I think of the hospital, where I’d usually be this time on a Sunday morning. Guilt arrives, tainting my pleasure.
This weekend is a “free” weekend. The first of many. Up until now, I’ve been responsible for the care of my patients admitted to G.R. Baker hospital. I work as a family doctor in a solo practice in Quesnel. For the past 20 years, apart from a couple of holidays here and there, I’ve been on duty every day. But recently I’ve resigned my admitting privileges. I will no longer be following my patients in hospital. Anxiety sets in.
Have any of my patients been admitted this weekend? Which designated doctor of the day is taking care of them? Are they okay?
I will only find out on Monday when I return to the office.
My sneakers crunch on gravel as I pass a yard cluttered with lumber, the shell of a rusted car, even a pair of tattered airplane wings, long-neglected projects now yard art.
Neglected. Another trigger. Do my patients feel abandoned? Do they think I don’t care for them anymore?
Stop it, Judy.
Wait! Too judgemental. Try again.
That’s curious, Judy. You’re having shame thoughts. Breathe. Notice the moment. A red canoe slithers past, the gentle splash of an oar propelled through water. The smell of ground quenched with melting snow. A crow caws a rebuke from a telephone wire and takes off to settle high on a blue spruce. Free.
I feel some shame thinking about how I plucked at my freedom, at the expense of my patients. But I have been here before. I have learned a thing or two about guilt and acknowledging one’s limits before burning out.
A decade before, one year before my 50th birthday, I made a difficult choice. I quit doing emergency shifts at our rural hospital.
This was the list I made to justify my decision:
- Pre-menopause has kicked your butt. You are only sleeping two, maybe three hours a night. An exhausted doctor is dangerous to her patients.
- Working six to eight 10 to 14-hour calls a month is unreasonable when you practice as a solo doctor.
- Working 80- to 100-hour weeks is dangerous to yourself and your patients.
- You already have 1,700 patients who need your care. A tired doctor will cause harm.
- You are not responsible for a system failure. It is the responsibility of the health authority to manage resources.
- You are one person, imperfect, but doing the best you can.
- Keep going at this pace, and you will be so burned out, you’ll self-combust.
A colleague warned me I’d get bored without the excitement of the ER. As if! I’d rotated through emergency rooms in three different continents. Decades of blood, guts and gore, panicked patients, desperate family members, tired and overworked nurses. Those savoured moments at the end of the shift when I realized no patient had died on my watch that day, feeling then as if I was taking my first breath in hours.
When I quit call, my working hours dropped to 40 maybe 50 hours a week. Heaven! For the first time in a long medical career, I’d had time. What to do?
My husband and I travelled some. I learned about and wrote about racism, poverty, violence and the forces that can tear a society apart. Writing courses, mentors, and my writing friends became a new chapter in my life. Not only was I taught more about white prejudice and white privilege, I was also led towards practicing trauma-informed care.
Writing, not medicine, taught me about complex post-traumatic stress syndrome. I learned that this condition explains my own anxiety, depression, ADHD, and personality quirks. It also explains why a loving father could hurt his children.
My father was six months old when his father dropped him and his four siblings off at an orphanage in Bethlehem, South Africa. He was beaten, abused, and taught his racist ways by the people who ran the institution, the Dutch Reformed Church. My father’s anxiety and PTSD turned into rage.
My mother’s trauma started in the womb. Mom was born in Holland during the Second World War. Her father was a German hiding from the Nazis because he refused to fight in the war. After the war, they came to South Africa for a better life, but my grandfather never recovered. He couldn’t provide, and my grandmother suffered. Mom grew up in poverty and without love, which made it difficult for her to nurture her children.
My siblings and I, coming of age in Welkom, South Africa, inherited the traumas of our parents and their parents. Adverse child events can be scored. Someone with a score of four or more on average lives 20 years less than someone with a score of less than two. Mine is six out of 10. All the more reason to pay attention to my health.
Learning about this condition has changed the way I practise medicine. It changed the way I think about myself. I replace self-blame with curiosity. When my leg beats faster than a Neil Peart drum solo, I’ll stop and say, “That’s curious, Judy, you’re anxious.”
Wings flutter in water and three pelicans glide into the air, coasting on thermals. Nearby, perched on long legs on islands of reeds or along the shore, large groups preen and puff out their feathers, their bodies snug against each other. I envy their serenity, their seamless togetherness.
Humans, too, are social animals, meant to interact. A 2009 academic survey of individuals over the age of 50 from 11 European countries found, unsurprisingly, that social participation improved health.
Why has it always been so hard for me to be comfortable around other people? I realize now that complex PTSD and its mate, social anxiety, are partly to blame. I’ve come to see, too, that working in a busy solo practice leaves little time or energy for socializing.
And so, in May, when our health authority decided to impose yet another load onto the shoulders of a select group of doctors, myself included, I quit my admitting privileges.
My first step to healing had been noticing my anxiety. The next will be forgiving myself for not working as hard as I had in my younger years.
The historian and philosopher Yuval Noah Harari discusses expectations in terms of imagined reality. In his book, Sapiens, he says: “Unlike lying, an imagined reality is something that everyone believes in, and, as long as this communal belief persists, the imagined reality exerts force in the world.”
In our rural community, family doctors are expected to accept an increased burden of care compared to city doctors. We share a gargantuan load of work: taking care of hospital patients; working 10- to 14-hour emergency shifts; helping mothers deliver their babies; looking after newborns; working as anesthetists; performing caesarean sections; managing patients with multiple diseases and serious medical conditions and patients with chronic pain and significant mental ill health — all with few resources.
When I decided I needed to take care of myself, as well, the decision to let go of my hospital care work was sweet sorrow. Sweet to not have to wake thinking immediately of having to care for seriously ill patients. Sorrow because I won’t be there to hold my patients’ hands when they need me. Until they’re discharged from hospital, another doctor will take my place. Maybe one they’ve never met.
I am concerned I won’t be at my patient’s bedside when they die. This is the hardest part for me. And for my patients. But in our community, we have wonderful community nurses who have helped me give my patients support, comfort, and pain relief when they die at home. My home visits will have to suffice. No guilt. No shame, Judy.
I am learning to accept my limitations.
I stop at the end of the road, at the turnaround. The flat tail of a beaver disappears below the water’s surface. A short distance away, four floating pelicans glide past.
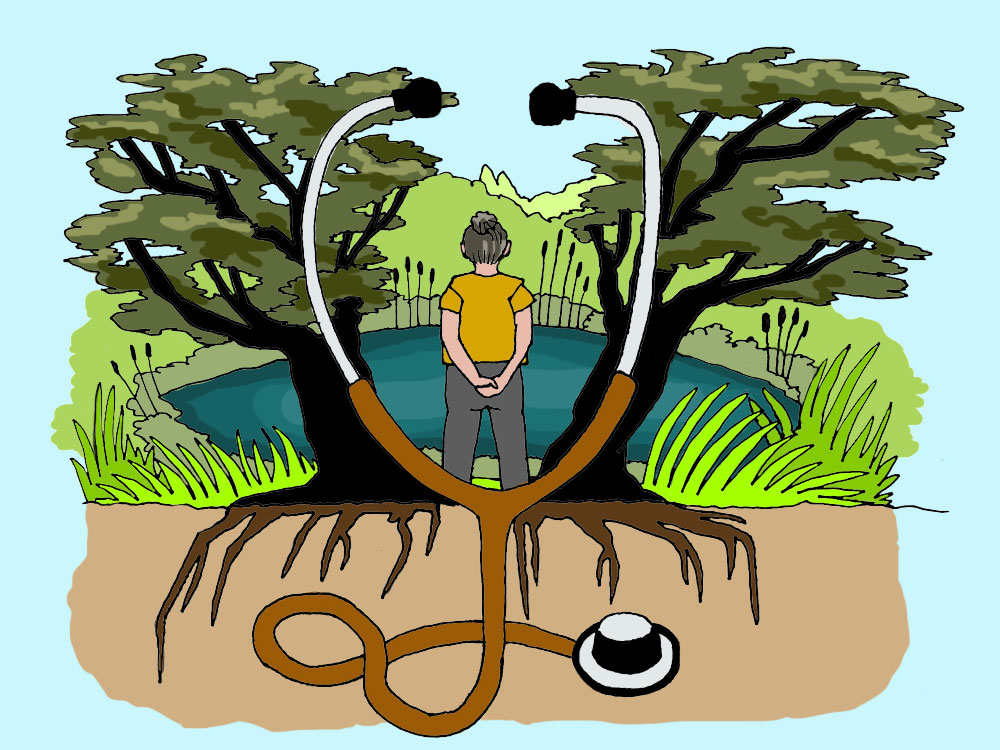
Healing surrounds me. I summon from my diaphragm and abdomen a breath that mutes the flight, fright, fight response that stirs within me. And then I turn around and head back home. ![]()
Read more: Health, Labour + Industry















Tyee Commenting Guidelines
Comments that violate guidelines risk being deleted, and violations may result in a temporary or permanent user ban. Maintain the spirit of good conversation to stay in the discussion.
*Please note The Tyee is not a forum for spreading misinformation about COVID-19, denying its existence or minimizing its risk to public health.
Do:
Do not: