“Emergency rooms are overflowing in BC. We’ve all seen the pictures.” — BC Liberal Party platform, 2001.
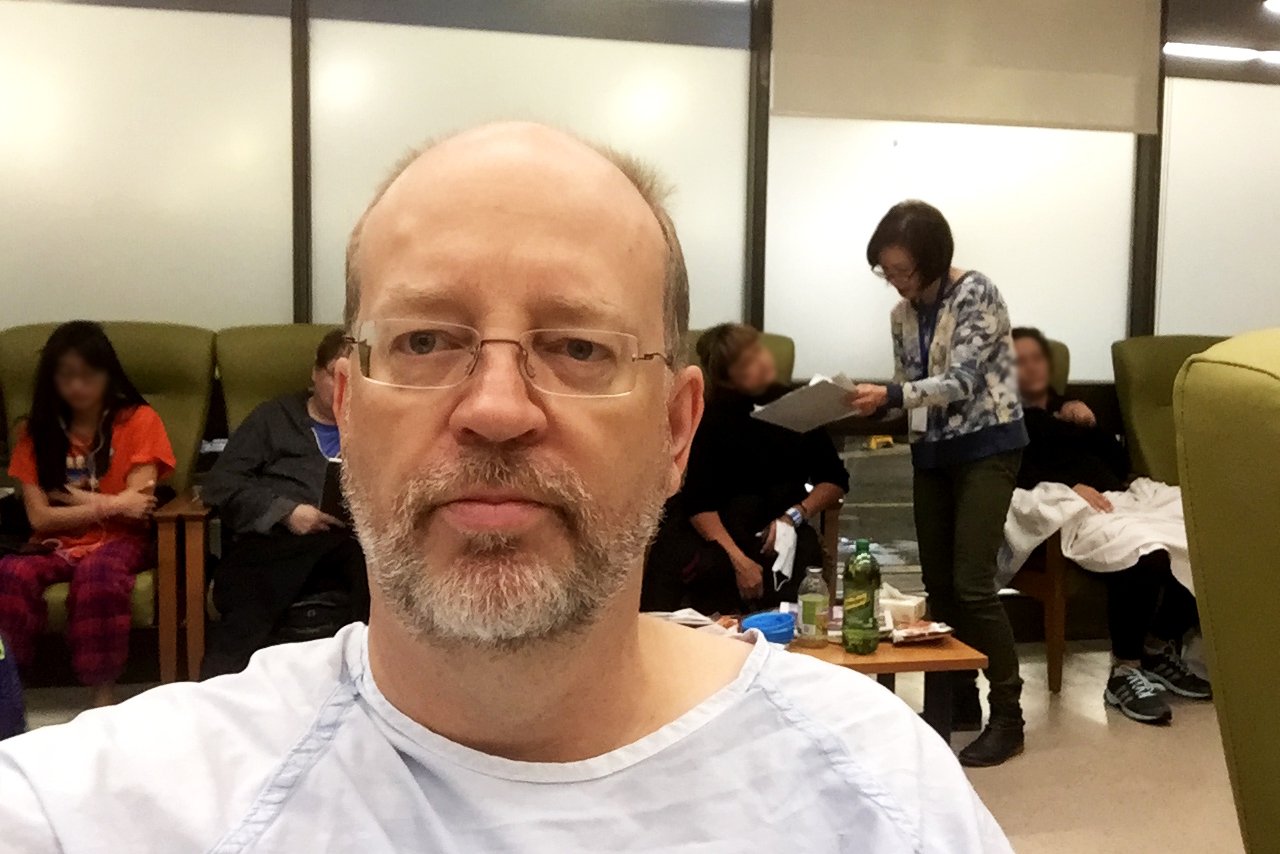
The chest pain was bad, I was short of breath, with a diagnosed heart condition, lying in bed in a hospital gown after an electrocardiogram test.
And then I was asked to leave Vancouver General Hospital’s emergency room — because they were out of space.
“I’m really sorry, but you have to go to the lobby waiting room — we have no space to treat other patients,” said the apologetic, embarrassed nurse last October. “Your clothes are in this bag and you can take your blanket. We’ll bring you back when we have a spot.”
I’d already been diagnosed with pericarditis — inflammation of the lining of the heart — 10 days earlier at VGH and the symptoms were back.
So while pericarditis is not a heart attack and rarely fatal, I was still stunned — as were six other patients asked to leave the triage area in the VGH emergency department and go out to the lobby in hospital gowns.
One of them was a retired teacher I know, who was in the ER after a previous surgery had appeared to result in an infection.
We sat together and talked about our astonishment that British Columbia’s biggest hospital and its major tertiary health care centre had to push patients in gowns, awaiting treatment, into the lobby. Fortunately, we were both able to re-enter the ER within 45 minutes.
Unfortunately, at least three patients recently died waiting for care in emergency rooms across B.C. — an unacceptable and tragic situation.
“I sat beside him, I held him, and I told him, I’m with you. I’m here.’ He took his last breath in my arms,” Janice Joneja wrote in a heartbreaking letter to Health Minister Terry Lake last month after her husband died of a heart attack in the waiting room of Kamloops’ Royal Inland Hospital before being seen by a physician.
Ironically, the man who died of cardiac arrest was Dr. Rajindar Joneja — a highly respected neurologist and psychiatrist who had served since 1968 in the hospital where he suddenly died.
“No one, regardless of their position, should pass from this life in such traumatic, public and obviously avoidable circumstances,” Janice’s letter continued. “That he should be consigned to a public waiting room to await the convenience of medical staff in the hour of his greatest need is unconscionable.”
Sadly, Joneja is just one of three tragic ER deaths reported in recent months. And while his death may have been unavoidable, others were not — and no one should die in the waiting room.
For Jennifer Whiteside, Hospital Employees’ Union secretary-business manager, the ER crisis is largely due to lack of provincial funding.
“It took 15 years to get to this emergency room problem — it’s going to take a long time to solve it,” Whiteside, whose union has members throughout VGH, said in an interview Sunday.
“Our per capita spending on health care in B.C. used to be number two and now we’re number eight. One of the results is overburdened emergency rooms.”
And while my situation in October never compromised my health, Whiteside said it shouldn’t happen.
“I would not want to be in that situation — I’m ill, I’m in a hospital gown and I’m in the lobby with the general public. That’s a serious problem that needs to be addressed. It doesn’t make sense,” Whiteside said.
Vancouver Coast Health Authority spokesperson Anne Marie D’Angelo agreed that moving patients in hospital gowns out of the VGH emergency into the lobby is wrong.
“Certainly it’s never appropriate for anyone to be put in a position of lacking dignity,” D’Angelo told me Friday, advising me to file a complaint with Vancouver Coastal’s Patient Care Quality Office, which I will do.
After being ordered from the ER, I was admitted to the cardiac care unit at VGH for five days with a severe case of pericarditis. (I am doing well and have been working, walking and living a mostly normal life since the beginning of 2017, so please don’t worry.)
And I have nothing but praise for the excellent team of cardiologists, doctors, nurses, hospital workers and other staff who took care of me at VGH. It is truly a remarkable cardiac care unit and hospital. But there is also no question that Vancouver General and other B.C hospitals have been stretched to the limit of their resources and beyond.
D’Angelo said at VGH and other emergency departments in Vancouver Coastal Health treatment priority is generally based on the patient’s condition.
“It’s to do with acuity, not first come, first served,” she said. “Emergency departments are busy places in all hospitals.”
Whiteside said part of the problem is the shortage of residential care and assisted living beds, which leaves patients waiting in hospitals beds. When hospital beds are full, patients fill emergency room spaces — and halls — and there is nowhere for new arrivals to be treated.
The growth in residential care beds has failed to keep up with demand, Whiteside said. “The need is increasing at a much faster rate than the number of beds available. It is a picture of declining assets.”
“We’ve seen an inability of health authorities to control the flow of patients in emergency rooms — they need to be admitted but there’s no beds,” she added.
The HEU believes privatization of health care has created more problems.
“There’s also a huge jump in residential private for-profit care — and there’s been a significant privatization as health authorities are starved for funds,” Whiteside said.
While D’Angelo of Vancouver Coastal isn’t complaining about funding, she added that, “We can always do more with more.”
Whiteside believes part of the solution is to give patients an alternative to ERs other than family doctors and walk-in clinics, which have limited hours.
“There’s an important role for community care clinics to play,” she said. “Integrated community care is needed.”
And it can’t come too soon for overextended hospital workers, doctors and nurses in ERs.
“Emergency rooms are a very complex environment to be working in — it’s very stressful with high work loads and more injuries,” Whitehead said. “I’ve been working with health care workers for over 15 years and the degree of stress in terms of injury rates, physical and mental exhaustion rates are very high.”
That stress and overwork results in sometimes tragic situations.
Surjit Kaur died in a wheelchair March 6 in New Westminster’s Royal Columbian Hospital emergency department, waiting for a bed to open up. Her family is angry she suffered an “undignified death” and waited for six hours without her vital signs being monitored or an intravenous line to replace fluids.
“She could’ve died with family around her and all the rituals that we do before somebody dies. She could have died like that if she had been taken care of,” said niece Amarjit Minhas.
Minhas herself is a former emergency room nurse.
“I’m just so sad that I work in a system where this kind of thing can happen. I worked in the ER 30 years ago, and things were bad then and there have been some improvements, but things are still as bad,” she told Global News.
Premier Christy Clark last month blamed “the flu season” for serious overcrowding at the Abbotsford Regional Hospital after nurses there described the emergency room as a “war zone.”
But the nurses pointed out that instead of the 88 required nursing positions in the ER, there were only 56 nurses on staff, with 32 positions unfilled. The “flu season” can’t be blamed for job vacancies.
Abbotsford Regional Hospital is where three-year-old Nimrit Gill tragically died in February of suspected pneumonia that went undetected in two visits to the ER in two days.
A patient safety review is underway, as is a BC Coroners Service investigation, but Nimrit’s grieving mother is clear about what she feels went wrong.
Balraj Gill told the Vancouver Sun that someone from Health Minister Terry Lake’s office contacted the family directly about the child’s death.
“He said they will look into it, what happened and why it happened so fast,” said Gill. “I said, ‘It’s not too fast. Five hours in an emergency room is too much time if you want to save a life.’”
After hearing about recent ER deaths, I definitely count my blessings at merely being uncomfortable.
But with 16 years in office, the BC Liberal government that promised better health care has no excuses for overcrowded emergency rooms where some patients sadly die before even being treated. ![]()
Read more: Health, BC Politics















Tyee Commenting Guidelines
Comments that violate guidelines risk being deleted, and violations may result in a temporary or permanent user ban. Maintain the spirit of good conversation to stay in the discussion.
*Please note The Tyee is not a forum for spreading misinformation about COVID-19, denying its existence or minimizing its risk to public health.
Do:
Do not: