In one week last month, paramedics responded to 494 suspected drug overdoses in Greater Vancouver, including 271 in the Downtown Eastside and 81 in Surrey. These numbers are not just alarming, but becoming alarmingly routine.
That was just one week in an ongoing opioid epidemic that has killed unknown thousands across North America this year. Even the U.S. Centers for Disease Control can’t offer a national estimate for 2015 or 2016; it says “Opioids were involved in 28,647 deaths in 2014 and opioid overdoses have quadrupled since 2000.”
That puts U.S. opioid deaths in the same class as firearms deaths, which have run around 30,000 a year since at least the 1960s. And like gun deaths, opioids are now a public health crisis we are stubbornly refusing to recognize.
Suppose those 494 overdoses in one November week had been cases of Ebola. B.C. Health Minister Terry Lake would have thrown more than $5 million at the problem, and his requests for help from Ottawa would have brought in many millions more.
And he’d need all the help he could get, because in the West African Ebola outbreak of 2013 to 2015, first responders and health care workers were among the disease’s victims — just as Toronto doctors and nurses were when SARS hit in 2003. (Vancouver escaped Toronto’s fate only because one nurse at Vancouver General Hospital read the Hong Kong media and alerted her colleagues when the hospital’s first SARS case turned up; the patient went into isolation.)
Never lose your first responders
Outbreaks only get worse when they also pick off the first responders, as West African health care workers learned; even those who escaped infection were deeply stressed, and many left the profession. We risk a similar experience if we take our own first responders for granted in this ongoing opioids epidemic.
Vancouver’s first responders risk death just being in the same space with opioids like fentanyl and the even deadlier carfentanil. Accidental ingestion at an overdose site, or absorbing such drugs through the skin, can be fatal.
Their training, so far, seems very adequate for the threat. In an email to The Tyee, Capt. Jonathan Gormick, public information officer of Vancouver Fire and Rescue Services, said:
“Vancouver Fire and Rescue Services use an array of personal protective equipment at all prehospital care calls, including medical gloves, protective eyewear, an N95 mask and if needed, a gown and face shield. Our staff all have at least First Responder licences from the EMA [Emergency Medical Assistants] Licensing Board, which involves 44 hours of training, with relicensing every three years.
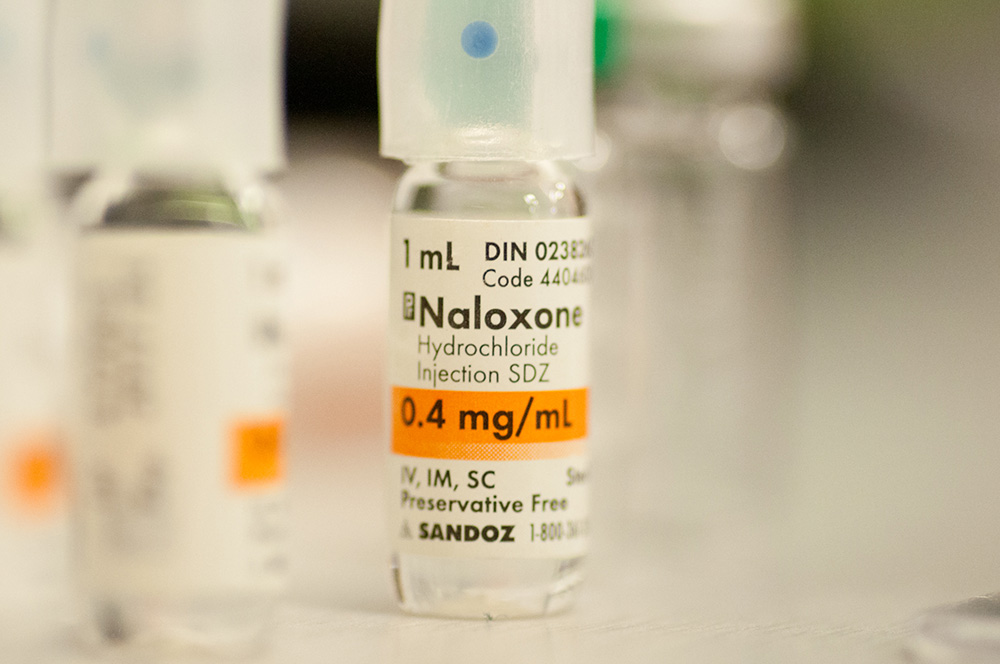
“We also undergo training for several additional patient care skills such as pulse-oxymetry, blood pressure, and course the three-four hour naloxone delivery training module. Although naloxone is the first injectable drug we have been authorized to deliver, part of our existing training covers the safe handling of sharps (used needles) and working around bodily fluids.”
Naloxone, meanwhile, is being promoted as something everyone should carry in overdose-prone neighbourhoods. So fire and rescue could arrive at an overdose scene and find that buddies have given the victim several doses. Gormick says his people “are authorized to deliver two 0.4 mg doses of naloxone, five minutes apart and regardless of any naloxone delivered by bystanders.”
First responders are trained to assess an overdose case, Gormick told The Tyee.
“The signs and symptoms that indicate naloxone use include: altered level of consciousness, bystander information regarding opiate use, signs of drug use, myosis, and respiratory failure or distress,” he explained. “Fortunately, naloxone has virtually no contraindications, and if the above signs and symptoms are due to another medical condition and not opiates, the naloxone has no negatives or side effects.”
Until recently, Vancouver Fire and Rescue personnel on an overdose call had to phone Emergency Physician Online Support and report the case to the on-duty physician. This was to get a kind of second opinion, but the requirement has very recently been dropped; firefighters, like any bystander, can now administer naloxone without delay.
But even the best-trained responders pay a price, Dustin Bourdeaudhuy, vice-president of Vancouver Fire Fighters’ Local 18, told The Tyee.
“I would start by saying that even though overdoses have been a part of the type of emergencies we have responded to for decades, we have never seen anything quite like this before. The sheer volume of people overdosing, in particular in the Downtown Eastside, is staggering. In a matter of months the overall call volume at the firehall that services that part of the city has gone from 600 calls per month to around 1,200. For the most part all due to the fentanyl crisis,” Bourdeaudhuy said.
‘The stress is wearing visibly’
“Obviously this takes a toll mentally and physically on everybody working down there,” he said. “Seeing people on the verge of dying repeatedly throughout your day and in some cases the same people overdosing on back-to-back days is hard to comprehend for anybody. The stress is wearing visibly on our staff and we are at a breaking point on how much volume of these calls the current number of firefighters staffed at that hall can bear.”
The number of overdose calls is affecting responses to all emergencies, Bourdeaudhuy said.
“The high volume of overdose calls is also affecting our depth of response. We are tied up at all these overdoses, so we are not available to respond to other emergencies such as fires. Resources are having to be pulled from other areas in the city, taking more time to respond and leaving those areas without that same level of protection.”
Fire and rescue, paramedics, and police — not to mention emergency department physicians and nurses — all need more financial, logistic and psychological support to deal with the opioid epidemic. Unlike infectious diseases like Ebola, this epidemic seems unlikely to burn itself out for lack of victims. New addicts will be recruited, new drugs concocted, whether in local labs or imported from China. A sophisticated delivery system is clearly in place across North America.
But even as we strengthen our first responders, we need to study addiction itself as a problem in human physiology, psychology and culture. A century of simple-minded moralizing about drugs, and criminalizing addicts, has brought us to this sorry state. We need to sabotage the whole underground drug economy by depriving it of its captive market.
If we don’t, our first responders — and we ourselves — will pay a heavy price for our failure. ![]()
Read more: Health















Tyee Commenting Guidelines
Comments that violate guidelines risk being deleted, and violations may result in a temporary or permanent user ban. Maintain the spirit of good conversation to stay in the discussion.
*Please note The Tyee is not a forum for spreading misinformation about COVID-19, denying its existence or minimizing its risk to public health.
Do:
Do not: